Abstract
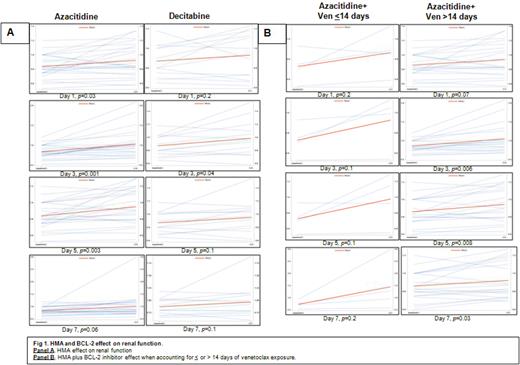
Background: Hypomethylating agents (HMA), such as azacitidine (AZA) /decitabine (DAC) plus BCL2 inhibitors are increasingly used as acute myelogenous leukemia (AML) therapy. However, side effects such as neutropenic fever, tumor lysis syndrome and acute kidney injury (AKI) are described. Although AKI induced by HMAs is infrequent, severity can result in permanent renal damage. Previous reports suggest that kidneys clear more than 50% of AZA with renal tubular acidosis and electrolytes abnormalities developing after drug exposure. To date, it is unknown whether concurrent comorbid conditions increase risk of AKI in AML patients. This study aimed to evaluate renal function overtime in patients receiving a HMAs plus venetoclax to determine each agent's ability to induce AKI. Methods: A single center retrospective, descriptive study from January 2018 to March 2022 was conducted at Baylor St. Luke's Medical Center. Patients with a confirmed diagnosis of AML, who received at least 1 cycle of venetoclax and a HMA, who were not eligible for intensive chemotherapy were included. Primary objective was incidence of AKI in AZA vs DAC during first week induction. Given potential additive impact of BCL2 inhibition on renal function, secondary objective was a subgroup analysis of patients in AZA group receiving venetoclax ≤ or >14 days. Descriptive and paired-t-test comparing baseline and daily sequential creatinine and glomerular filtration rate (GFR) were analyzed using SAS. Results: 40 AML patients were included. 25/40 (62.5%) and 15/40 (37.5%) received AZA and DAC. Baseline patient characteristics were well balanced between groups, except for differential absolute lymphocyte count (ALC) expression [3.4 K/uL vs 1.3 K/uL, in AZA treated vs DAC, p=0.01]. Patients receiving AZA developed significantly higher incidence of AKI from day 1 to day7. DAC was associated with transient significant AKI detectable only during day 5 (Fig 1A). At last follow up, incidence of irreversible renal failure was observed in 1/40 (2.5%) of AML patients. In further subgroup analysis, we sought to understand the possible nephrotoxic BCL2- inhibitor effect while combining with AZA. Patients exposed >14 days of BCL2- inhibitors developed sustained AKI throughout day 3 to day 7 [p=<0.05 for all time points], as compared to those receiving ≤14 days. No detectable differences on incidence of diabetes, heart failure, infections, and use of diuretics were found in patients exposed or not to 14 days of BCL-2 inhibitor. Conclusions: Our study demonstrates more severe and sustained worsening renal function in patients exposed to AZA than those receiving DAC. While our report recapitulates similar previous observations, we describe an important synergistic BCL-2 inhibitor effect on renal function when combined with AZA. It would be interesting to investigate whether higher than expected ALC cooperates to induce renal damage via enhanced T-cell immunity.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal